From A Silent Dance To A Metabolic Mambo
Every meal we eat, every move we make, intertwines with insulin’s silent dance within us—a hormone crucial for turning food into fuel. This intricate and essential dance has faced new challenges as our diets and habits have evolved over generations. Insulin, once a mere background player in our body’s complex biology, now takes into the spotlight as we confront rising diabetes and other metabolic conditions. The story of insulin resistance—a condition where our body’s response to insulin weakens—is not just a medical tale; it’s a call to action, encouraging us to rethink our relationship with our bodies and our environments.
At its core, insulin’s role is simple yet profound: it helps our cells absorb glucose, the sugar that fuels our activities, from the energy we need for things as common as thinking to the power required for running. But when insulin signals go unanswered by our cells, the fallout affects more than just our blood sugar levels. It’s a wake-up call that echoes through the halls of our arteries, muscles, and minds, contributing to a host of modern health dilemmas.
This post offers more than just insight into a hormonal hiccup. It’s a roadmap to resilience, showing how we can bolster our bodies’ response to insulin through mindful eating, regular physical activity, and an awareness of our metabolic health. This journey is about transforming knowledge into power—the power to shape our health destiny, nurture our well-being, and rediscover the harmony between lifestyle and biology. It’s a metabolic mambo!
Before We Knew Insulin
Once upon a time, in the heart of ancient Eastern lands, a mysterious condition called ‘honey-like urine’ captured the imagination of healers and scholars alike, marking the beginning of a quest for understanding. This condition was associated with frequent urination and sweet-tasting urine. The ancient Greek physician Aretaeus described the condition as a "melting down of flesh and limbs into urine." The early Greeks coined this condition ‘diabetes,’ meaning ‘to go through’ or ‘siphon’ based on the hallmark signs of excessive urination at all times of the day. The condition was remarkable also for the excessive thirst and emaciation of those who suffered from diabetes.
For most of human history, our only understanding of insulin’s role in human health was based on observing the effects of its absence. It took three millennia to understand glucose metabolism and the existence of insulin, but eventually, humanity and science unpacked this mystery mainly through a condition called diabetes mellitus.
The discovery of the pancreas's role in glucose metabolism was established at the end of the 19th century, and we owe the discovery to dogs. Two physiologists removed the pancreatic tissue of dogs in a lab and observed glucose spilling into the urine, a hallmark sign of diabetes called glycosuria (sugar in the urine). A small series of experiments on these lab animals revealed to humanity what was largely unknown up until then for thousands of years. The pancreas controls the balance of glucose in the human body. These experiments in the late 1800s set the stage for the ensuing discovery of insulin about thirty years later.
In the 1920s, a young medical student named Charles Best was recruited by Frederick Banting, a Canadian surgeon, to work on extracting the mystery hormone from the pancreas of lab canines. The scientists carefully removed the pancreas of the lab dogs, still keeping them alive. Of course, the dogs developed diabetes. The proof of concept for the most primitive form of insulin was made by crushing the excised pancreas of lab animals, distilling it in saline, and infusing it back into the dogs whose pancreas had recently been removed.
After a small-volume infusion of a crushed pancreas cocktail, the scientists observed a drop in the dogs' glucose levels. Eventually, this team, working under the lab of Professor John Macleod at the University of Toronto, extracted and purified the peptide hormone we now know as insulin. In 1923, Frederick Banting and John MacLeod were awarded the Nobel Prize in Medicine for discovering insulin.
The impetus for the discovery of insulin was a search for a cure for those who could not produce insulin to metabolize glucose. A condition we now call Type 1 Diabetes. The life spans of these individuals were short, and they often died very young despite engaging in treatment protocols restricting food intake to prolong their lives. Isolating insulin and its iterations as an injectable medication has since saved countless lives. Ironically, in the 21st century, insulin is best known as a driver of disease and mortality due to its excess presence in the human body.
The Biology of a Bite
Navigate a culinary thread that begins with a simple act: eating a beef sandwich on sourdough bread. This journey is not just about savoring flavors or quelling hunger; it’s a ripple of complex biology, where every bite sets off a cascade of events far beyond what the eye can see.
As the sandwich meets your lips, the initial crunch of sourdough’s crust gives way to the tender succulence of beef, a fusion of textures and tastes that signals the start of a voyage. Chewing breaks down the bread and beef, mechanically tearing apart fibers and mixing them with saliva. Enzymes in saliva, like amylase, begin the breakdown of carbohydrates in the sourdough into simpler sugars, a hint at the intricate dance of digestion and metabolism about to unfold.
Swallowed bites find passage down to the stomach, where acids and enzymes further dismantle the meal into its nutrient constituents: amino acids from beef, simple sugars from bread, and fatty acids from both the meat and any added condiments. This nutrient-rich slurry then enters the small intestine, the stage where most nutrient absorption occurs. It’s here that insulin enters the narrative.
As glucose levels rise from the digested sourdough, the pancreas releases insulin as the key master of this biological matrix. Insulin is the key that unlocks the door to our body’s cells, allowing glucose to enter and be used as fuel. Imagine insulin as a messenger, darting from cell to cell, whispering the secret code that unveils vast energy reserves previously out of reach. Muscle cells rejuvenated, brain cells invigorated—each bite of the sandwich translating into energy and nourishment, thanks to this hormonal guide.
But insulin's role extends beyond unlocking energy from glucose. It also aids in storing excess nutrients, ensuring our body can tap into reserves when needed. The amino acids from beef, now building blocks for repairing and building tissues, are ushered into cells under insulin’s watchful eye. Fatty acids, too, find their destinations and are stored for future energy needs.
This molecular and hormonal cascade set in motion by a simple beef sandwich on sourdough bread is a marvel of biology, a reminder of the intricate systems at work within us. Every meal ignites this dance of nutrients, hormones, and cells, a journey from plate to physiology that sustains life’s essence.
Understanding the journey of our food, from bite to biology, gives us a deeper appreciation for the meals that nourish us and the incredible efficiency of our bodies in harnessing their nutrients. It’s an unlocking of unseen yet indispensable processes that power every thought, movement, and breath.
Insulin & Resistance
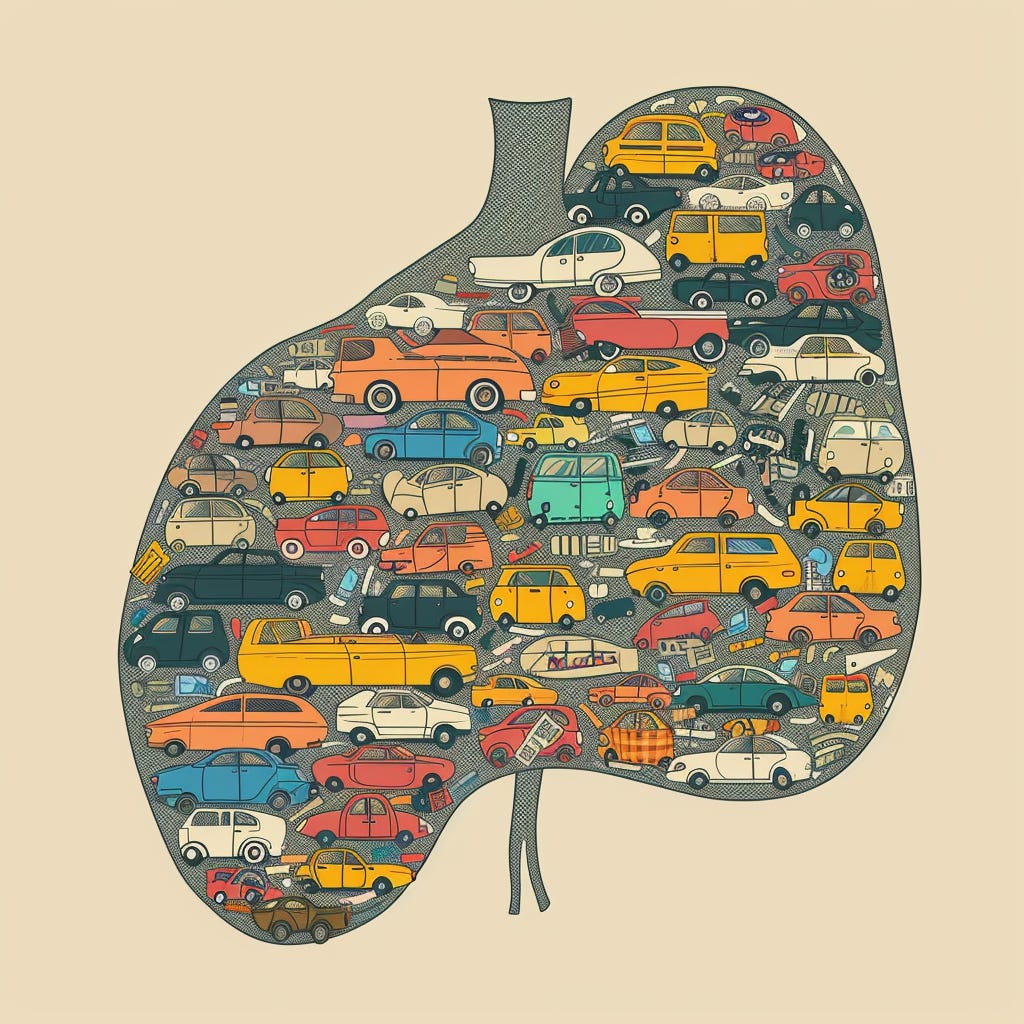
Insulin resistance is like a miscommunication in the body's system for managing sugar levels, leading to various health problems. Imagine your body as a bustling city where insulin is the key that opens doors to allow sugar from the blood into cells for energy. When insulin resistance sets in, it's as if these keys are not working correctly, leaving too much sugar in the bloodstream instead of getting into the cells where it's needed.
At the heart of this issue are complex cellular mechanisms. Typically, when insulin attaches to a cell, it starts a chain reaction inside the cell to let sugar in. However, with insulin resistance, this process breaks down. It might be due to a glitch in the insulin receptor, issues with specific molecules that help signal inside the cell, or problems with the mechanisms that move sugar into the cell.
Adding to the complexity, factors like lipotoxicity and glucotoxicity worsen the situation. Lipotoxicity occurs when fats and excessive sugar in the blood interfere with insulin's job. Think of it as traffic jams and roadblocks in our city, preventing insulin from reaching its destination. Accumulation of lipids within non-adipose tissues like the liver and muscle can interfere with insulin signaling, a phenomenon known as lipotoxicity. Similarly, chronic high glucose levels (glucotoxicity) can impair insulin signaling and beta-cell function.
Chronic low-grade inflammation is closely linked to insulin resistance. Chronic inflammation is like a city under constant stress from pollution, which disrupts insulin's signaling pathways. Inflammatory cytokines can interfere with insulin signaling. Adipose tissue, particularly in obesity, can become inflamed and produce cytokines (signals from cells) and other substances that promote insulin resistance.
Similarly, when the endoplasmic reticulum (a cellular component responsible for protein folding) is overwhelmed, it's akin to a factory within the city shutting down, contributing to the breakdown in insulin signaling.
An overloaded system can lead to ectopic fat storage, where fat accumulates in places like the liver and muscle, much like when a city runs out of parking spaces and cars start parking in unauthorized areas, causing chaos.
Hormonal changes also impact insulin resistance. Just as the economic balance of a city can be affected by the rise and fall of specific industries, the balance of hormones like adiponectin and resistin can affect insulin sensitivity.
Genetics, diet, lifestyle, and other factors like mitochondrial dysfunction, hyperinsulinemia, oxidative stress, and altered fat metabolism are akin to the various infrastructure, policies, and environmental factors that influence a city's health and efficiency. Additionally, the complex interaction between different organs, changes in the gut microbiota, and various circulating metabolites and hormones illustrate the interconnectedness of the city's systems and the delicate balance required to maintain health.
In essence, insulin resistance is the result of a multifaceted breakdown in the body's ability to manage sugar, influenced by a range of genetic, lifestyle, and environmental factors, much like the health and functioning of a city are influenced by a complex interplay of systems, policies, and environmental conditions. Understanding and addressing these factors is crucial for restoring balance and ensuring the efficient management of sugar in the body.
Signs of Insulin Resistance
Insulin resistance is a stealthy condition, often creeping up unnoticed and laying the groundwork for more serious health issues like prediabetes and type 2 diabetes. Its symptoms are subtle, easy to overlook, and sometimes don't make themselves known until the situation has escalated. Yet, knowing what to watch for can be the key to early detection and management. Let's delve into the signs and symptoms that could indicate insulin resistance, breaking down complex medical terms into understandable insights.
One of the first potential indicators of insulin resistance is a condition known as Acanthosis Nigricans. This might sound complicated, but it's essentially areas of dark, velvety skin that often appear on the back of the neck, in the groin, or under the arms. Imagine the skin getting thicker and darker, almost like it's been brushed with velvet. This change can be a visual clue that something's wrong with how your body is processing insulin.
Another sign to look out for is the appearance of skin tags. Small, soft, skin-colored growths tend to pop up where your skin folds or rubs together. Though skin tags are generally harmless on their own, their presence can be a marker of insulin resistance, especially when many of them exist.
Then, there's the matter of increased waist circumference. It's a bit more straightforward: men with a waistline over 40 inches and women with one over 35 inches may have insulin resistance. This measurement isn't just about fitting into your pants; it's a significant indicator of health concerns related to insulin processing in your body.
High blood pressure is another sign that shouldn't be ignored. Readings of 130/80 mmHg or higher can indicate your body struggles with insulin resistance. High blood pressure is like a warning bell, telling you that your heart and arteries are under more strain than they should be.
Abnormal blood lipid levels also play a role in signaling insulin resistance. This includes a fasting triglyceride level over 150 milligrams per deciliter (mg/dL), an HDL cholesterol level under 40 mg/dL in men, and under 50 mg/dL in women. These numbers represent the balance of fats in your blood, and when they're out of whack, it's a sign that insulin isn't doing its job correctly.
Elevated blood sugar levels are the most direct indicator of insulin resistance. A fasting glucose level at or above 100 mg/dL or a blood sugar level at or above 140 mg/dL two hours after a glucose load test suggests that your body has difficulty managing sugar levels, an essential insulin function.
Finally, an elevated A1C level is another red flag. This percentage reflects your average blood sugar levels over the past 2-3 months, providing a broader view of how well your body manages glucose.
While insulin resistance might initially fly under the radar, knowing these signs can help you catch it early. If you notice any of these symptoms, it's crucial to consult with a healthcare professional for advice and potential intervention. Early action can make a significant difference in managing insulin resistance and preventing it from progressing to more serious conditions. Understanding these signs is the first step toward taking control of your health and ensuring your body's insulin is working effectively.
Roadmap to Resilience
The great thing about building resilience in your metabolism is that there is more than just one way. There is no one size fits all, there are many small paths that converge synergistically that can get you to your destination. Covering them all is a book, so in this post we will cover a handful.
Moving Day, Everyday
In a 2014 study focusing on the impact of walking exercises on obese women, significant findings point to the effectiveness of moderate aerobic activity in combating obesity and its associated metabolic disorders. Over 12 weeks, participants engaging in tailored walking sessions saw reductions in abdominal fat but also experienced improved insulin resistance and serum cytokine levels. This research underscores the importance of physical activity, particularly walking, as a manageable, non-invasive method for improving health outcomes in obese women. By dedicating just a few hours a week to moderate walking, participants witnessed tangible health benefits, marking a significant step forward in the fight against metabolic syndrome and obesity-related inflammation.
A 2013 study published in PLOS ONE reveals that substituting sitting time with minimal-intensity activities like standing and walking has more profound health benefits than shorter bouts of moderate to vigorous exercise, such as cycling. The research emphasizes the effectiveness of longer-duration, low-intensity physical activities in improving insulin sensitivity and plasma lipid profiles, even when energy expenditure remains constant.
Integrating longer periods of low-intensity activities, such as standing and walking, into our daily routine can counteract the harmful effects of sitting and provide substantial health benefits. This insight is particularly relevant in today’s sedentary lifestyle, suggesting a shift towards more active living, even at minimal intensities, can lead to a healthier life.
The simplicity of standing and walking as forms of physical activity makes this a feasible and accessible health strategy for most people, highlighting the need to reevaluate our daily routines for better health outcomes.
The Outside Within
We don’t really think of our intestinal tract (GI tract) as being outside of us, but it is. The GI tract is a hollow tube that travels through us and represents an interface between the outside world and that which lies deep within. In the quest to understand and combat insulin resistance scientists are turning their gaze to this interface, specifically to the gut microbiome. This thriving ecosystem inside our digestive tract, home to trillions of microorganisms, is emerging as a key player in the development of insulin resistance, and potentially, type 2 diabetes.
A Delicate Balance
Research reveals a fascinating insight: the balance of bacterial species in our gut, including groups like Firmicutes, Actinobacteria, and Bacteroidetes, correlates with our metabolic health. Disruptions in this balance can increase intestinal permeability, allowing harmful substances to enter the bloodstream, provoke inflammation, and disrupt insulin signaling pathways.
The Potential of Probiotics and Prebiotics
The spotlight is on probiotics—live beneficial bacteria found in fermented foods—and prebiotics, dietary fibers that feed these good bacteria. Studies suggest that specific probiotics containing strains of Lactobacillus and Bifidobacterium may improve insulin sensitivity. However, human trials show mixed results, underscoring the need for further investigation.
Prebiotics, on the other hand, are shown to favorably alter the gut microbial landscape, promoting metabolic health and offering a potential tool against insulin resistance. Combining probiotics and prebiotics into synbiotics could synergistically enhance insulin sensitivity by modulating the gut microbiota and reducing inflammation.
Fast Life, Slow Metabolism
Fast food often replaces balanced meals and moving the body might take a backseat to the constant demands of life. It's no wonder insulin resistance is more pervasive than we realize. But what if the path to better health and combating this growing concern lies not in the pharmacy but in the garden? Natural compounds, especially those derived from plants, are stepping into the spotlight for their potential health-boosting benefits, including their ability to fight against insulin resistance. Let's delve into the details of some remarkable plants and the research surrounding their extracts.
The Mighty Morus alba L. (White Mulberry)
Imagine a plant so powerful that it can slow down the absorption of sugar in your blood. That's the magic of the White Mulberry tree. It contains a compound called 1-deoxynojirimycin (DNJ) that acts like a superhero, blocking an enzyme involved in digesting carbohydrates. This means glucose enters your bloodstream at a slower pace, potentially improving your body's sensitivity to insulin and reducing insulin resistance.
Sacha Inchi's Secret
Sacha Inchi, also known as the Inca peanut, is not just another nut. It's rich in alpha-linolenic acid, a type of omega-3 fatty acid, and packed with antioxidants. Preliminary studies are whispering exciting news about its ability to polish up lipid profiles and possibly enhance insulin sensitivity. However, these whispers need to grow into loud conversations with more research to confirm its effects on insulin resistance.
Tribulus Terrestris: More Than Just a Libido Booster
Traditionally celebrated for boosting sexual function and increasing testosterone levels, Tribulus Terrestris might also be a secret weapon against high blood sugar levels. Animal and human studies hint at its potential to improve insulin sensitivity, but the jury is still out on its effects in humans, calling for more research to get the full picture.
Puerarin: Kudzu Root’s Gift
Puerarin, an isoflavone from the Kudzu root, could be a game-changer for those facing cardiovascular issues and insulin resistance. It's thought to help by enhancing how glucose is taken up and used by the body. Although the science is still in the early stages, and more human studies are needed, the potential benefits of Puerarin look promising.
Pomegranate: More Than Just a Tasty Treat
Pomegranates are not only delicious but may also be a potent ally in improving insulin sensitivity and reducing blood sugar levels, thanks to their antioxidant-packed extracts. But there’s a twist. The effect is best when coupled with exercise. Of course, no juice packed with glucose or fructose is likely to help insulin resistance. The combination of pomegranate juice (without sugar!) and aerobic exercise led to the greatest improvements in fasting blood sugar, insulin levels, and insulin resistance index (HOMA-IR). Liver enzymes AST, ALT, and GGT, which are often elevated in diabetes, were also significantly lowered.While the fruit holds promise, further research is needed to fully understand its role in managing insulin resistance.
These natural wonders offer a hopeful glimpse into managing insulin resistance and related metabolic disorders through improving insulin sensitivity, enhancing glucose uptake, reducing oxidative stress, and modulating lipid metabolism. However, it's crucial to approach them with caution. The encouraging results from preclinical studies need to be backed by rigorous clinical trials to confirm their safety and effectiveness. Moreover, consulting healthcare professionals before trying these natural compounds is essential, especially for those with existing health conditions or on medication, to avoid potential interactions and side effects. In the quest for health, the natural world continues to offer intriguing possibilities, blending ancient wisdom with modern science.
Unlock the Possibilities, Embrace the Journey
As we delve deeper into the intricate dance of insulin within our bodies, we're reminded of the power we hold to shape our health destiny. From the silent workings of a single hormone to the complex interplay of lifestyle, genetics, and environment, the story of insulin resistance is a call to action—a reminder that our well-being is a journey, not a destination.
The path to metabolic resilience is paved with small, consistent choices. It's in the simple act of taking a walk, the mindful selection of nutrient-rich foods, and the exploration of natural compounds that may hold promise. It's in the understanding that our gut microbiome is a vital partner in this dance, and nurturing its balance can have profound effects on our insulin sensitivity.
But the journey is not without its challenges. In a world where fast food and sedentary lifestyles have become the norm, it takes conscious effort and commitment to break free from these patterns. It requires a shift in perspective, a willingness to prioritize our health, and a curiosity to explore new avenues of well-being.
The science surrounding insulin resistance is evolving rapidly, offering new insights and potential solutions. From the promise of probiotics and prebiotics to the intriguing effects of natural compounds like White Mulberry and Puerarin, researchers are unraveling the complexities of this condition and paving the way for innovative approaches to management and prevention.
Yet, it's crucial to approach these discoveries with a discerning eye, recognizing that while the potential is vast, the journey from lab to real-life application requires rigorous testing and personalized guidance from healthcare professionals.
In the end, the story of insulin resistance is a story of empowerment. It's a reminder that our health is not determined solely by the cards we're dealt, but by how we choose to play them. By embracing the dance, by making small, consistent steps towards metabolic resilience, we can transform the silent struggle into a vibrant celebration of well-being.
So let us step onto the dance floor, armed with knowledge, curiosity, and a commitment to our health. Let us find joy in the journey, knowing that every choice we make is a step towards a more vibrant, resilient future. The music of our metabolism is playing, and it's up to us to find our rhythm.
Dr. Hector Caraballo, MD, is a physician who gained invaluable insights into the art of healing and medicine through his own life-changing health crisis. In today's fast-paced world, Dr. Caraballo emphasizes the importance of mastering 'The Medicine of You', an approach that invites individuals to become data-driven about their health markers that can impact both lifespan and healthspan. Through his writing, he aims to empower people to take control of their health before a significant crisis occurs, using his own experience as a gift to help others navigate the complexities of health and well-being. Dr. Caraballo is the founder of Vital Essence Medica, an online medical consultation service leveraging regenerative, personalized, and functional medicine. He also serves as the Medical Director of IV Essence in San Antonio, Texas.